The blood-brain barrier (BBB) is a vitally important gatekeeper of sorts that protects the brain and central nervous system (CNS) from pathogens and potential neurotoxins, whilst allowing the transport of nutrients, salts, proteins, and certain other substances into the brain and CNS.
In this article, we will discuss what the BBB is, how it is structured, how its health and optimal function are maintained, and also how it can be compromised by medications and disease. If you already know about the BBB and want to learn about its interactions with GABA, specifically if GABA can cross the BBB to enter the brain, read here!
What is the blood–brain barrier?
The BBB represents both a physical as well as a metabolic barrier that isolates the CNS from the systemic circulation under normal conditions, providing a unique and stable environment for optimal neuronal function [1]. Without the BBB, the CNS is at risk of invasion of toxins, pathogens, immune cells, or ion dysregulation, which could lead to neuronal dysfunction and degeneration.
The BBB has two-way control over the transport of a large and diverse range of regulatory proteins, nutrients, and electrolytes (i.e., salts), as well as potential neurotoxins. This traffic is policed through several different transport mechanisms [2,3]. The BBB defends the CNS by using efflux transporters that block intravascular toxin entry and promote the elimination of toxic substances in the bloodstream [3,4]. The barrier also selectively restricts the passage of peripheral immune factors, such as signaling molecules, antibodies, and immune cells, into the CNS, thus insulating the brain from damage due to peripheral immune events [5].
The nature of the BBB means that delivering therapeutic medications to specific regions of the brain is a huge problem, making the treatment of many brain disorders difficult [6]. Virtually all large-molecule neurotherapeutics and more than 98% of small-molecule drugs are excluded from the brain by the BBB [7]. This challenging phenomenon is an important avenue of ongoing and future research.
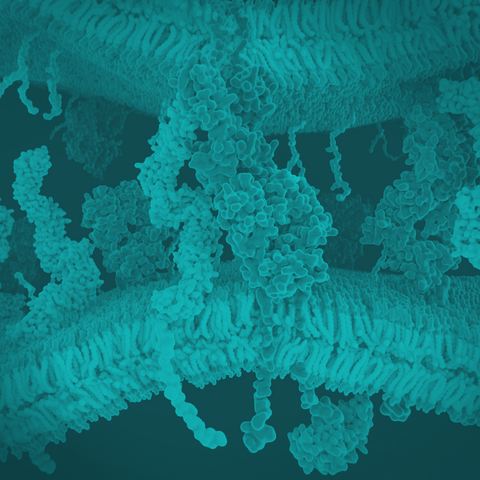
How is the blood–brain barrier structured?
The core anatomy of the BBB is the cerebral blood vessel formed by brain endothelial cells (ECs). ECs of the BBB are unique compared with ECs in different tissues as they have continuous intercellular tight junctions (TJs), lack fenestrations, and undergo extremely low rates of transcytosis, which greatly inhibits both the paracellular and transcellular movement of molecules through the EC layer [8]. This means that the passage of molecules through the BBB is selectively governed by a series of specific transporters, which allows the delivery of nutrients to the brain and at the same time prohibits potential toxins. In addition, ECs have low expression of leukocyte adhesion molecules, stopping immune cell infiltration into the healthy CNS, although there is immune surveillance to a limited extent.
The BBB exists at all levels of the vascular tree within the CNS, including the penetrating arteries and arterioles, the dense capillary bed, the post-capillary venules, and the draining venules and veins. Although each vascular segment needs to maintain tight barrier properties to insulate the neural tissue from the blood, there are specializations within the vascular bed that are crucial for BBB function. For instance, nutrient transport is highly specialized to the capillaries which come close to all the neurons, whereas regulation of leukocyte trafficking and immune modulation resides at the post-capillary venule where there is a perivascular space.
The development and maintenance of the BBB are governed by cellular and non-cellular elements that interact with the ECs. Astrocytes, pericytes, and extracellular matrix (ECM) components provide both structural and functional support to the BBB. The term "neurovascular unit" (NVU) additionally refers to neurons, microglial cells, and, optionally, peripheral immune cells that also contribute to this cellular interplay. The abluminal surface of brain capillaries is ensheathed by a basement membrane that separates ECs from pericytes, and pericytes from astrocytes. At the level of the post-capillary venule, the two basement membranes are distinct (endothelial and parenchymal) and define the inner and outer border of the perivascular space where bone marrow-derived perivascular cells have key immunoregulatory functions.
How can the blood–brain barrier integrity be compromised?
Perhaps unsurprisingly, barrier dysfunction (such as in neurological diseases or infections) can be life-threatening [9,10].
Barrier disruption is seen in many different neurological disorders including multiple sclerosis (MS), stroke, Alzheimer's disease (AD), epilepsy, and traumatic brain injuries [4]. Functional imaging of human patients and analysis of postmortem brain samples have identified the pathological breakdown of the barrier in different neurological diseases. In addition, research with animal models of disease and with cell culture BBB models has enabled the identification of some of the molecular mechanisms that cause changes to the BBB. This dysfunction can include alterations in many different properties of the BBB including TJs, transporters, transcytosis, and LAM expression. This breakdown can lead to edema, disruption of ionic homeostasis, altered signaling, and immune infiltration that can lead to neuronal dysregulation and, ultimately, degeneration. Although BBB dysfunction is often secondary to the primary insult in these diseases, in some cases, it has been a suggested cause, including MS, epilepsy, and AD.
Nearly all aspects of the BBB can be altered in BBB breakdown when compared to a healthy BBB [10,11]. The alterations and breakdown of functional components of the BBB can occur naturally with aging even in the absence of underlying conditions that cause cognitive decline and dementia [11]. The disruption that occurs in healthy aging may become more detrimental when exposed to a second component, such as inflammation for instance. Notably, the BBB may be disrupted in aged mice as shown by research, but cognitive decline is not apparent until there is an inflammatory challenge [12]. The morphological and molecular alterations of the BBB happen in the absence of disease pathologies.
Can the blood–brain barrier be restored?
The disruption of the BBB in neurodegenerative disorders makes it an obvious target for therapeutics. If BBB disruption could be restored, at least to a degree, it may be possible to slow the pathogenesis of a given disease. Tightening the barrier could reduce the negative effects of the inflammatory challenge or, in the presence of any of the neurodegenerative diseases, controlling the integrity of the BBB could slow the progression of the disease and neurodegeneration.
As an example, ischemic stroke inflicts damage upon the BBB, triggering adverse stroke outcomes such as cerebral edema, hemorrhagic transformation, and aggravated neuroinflammation. Effective repair of the damaged BBB after stroke and neovascularization that allows for the unique selective transfer of substances from the BBB after stroke is necessary and important for the recovery of brain function. Most new therapies show increased expression of BBB TJ proteins, and some show beneficial results in terms of enhanced pericyte coverage at the injured vessels [13].
Summary
This article has provided an overview of the role of the BBB, its structure and function, maintenance and development, and lastly how it may be compromised by drugs and disease. The function and structure of the BBB are vital to maintaining brain health and optimal function. The disruption of any of the functions of the BBB potentially leads to BBB breakdown or loss of integrity, thus putting brain homeostasis at risk. Deterioration of BBB form and function is a feature of healthy aging, but it is worsened in many neurodegenerative disorders and is a hallmark of cognitive decline.
References
[1] W.M. Pardridge, Molecular biology of the blood-brain barrier, Mol Biotechnol 30 (2005) 57–70. https://doi.org/10.1385/MB:30:1:057.
[2] N.J. Abbott, I.A. Romero, Transporting therapeutics across the blood-brain barrier, Mol Med Today 2 (1996) 106–113. https://doi.org/10.1016/1357-4310(96)88720-x.
[3] J. Correale, A. Villa, Cellular elements of the blood-brain barrier, Neurochem Res 34 (2009) 2067–2077. https://doi.org/10.1007/s11064-009-0081-y.
[4] R. Daneman, A. Prat, The blood-brain barrier, Cold Spring Harb Perspect Biol 7 (2015) a020412. https://doi.org/10.1101/cshperspect.a020412.
[5] L.L. Muldoon, J.I. Alvarez, D.J. Begley, R.J. Boado, G.J. Del Zoppo, N.D. Doolittle, B. Engelhardt, J.M. Hallenbeck, R.R. Lonser, J.R. Ohlfest, A. Prat, M. Scarpa, R.J. Smeyne, L.R. Drewes, E.A. Neuwelt, Immunologic privilege in the central nervous system and the blood-brain barrier, J Cereb Blood Flow Metab 33 (2013) 13–21. https://doi.org/10.1038/jcbfm.2012.153.
[6] M.D. Sweeney, A.P. Sagare, B.V. Zlokovic, Blood-brain barrier breakdown in Alzheimer disease and other neurodegenerative disorders, Nat Rev Neurol 14 (2018) 133–150. https://doi.org/10.1038/nrneurol.2017.188.
[7] D.S. Hersh, A.S. Wadajkar, N. Roberts, J.G. Perez, N.P. Connolly, V. Frenkel, J.A. Winkles, G.F. Woodworth, A.J. Kim, Evolving Drug Delivery Strategies to Overcome the Blood Brain Barrier, Curr Pharm Des 22 (2016) 1177–1193. https://doi.org/10.2174/1381612822666151221150733.
[8] B. Obermeier, R. Daneman, R.M. Ransohoff, Development, maintenance and disruption of the blood-brain barrier, Nat Med 19 (2013) 1584–1596. https://doi.org/10.1038/nm.3407.
[9] A. Patabendige, D. Janigro, The role of the blood-brain barrier during neurological disease and infection, Biochem Soc Trans 51 (2023) 613–626. https://doi.org/10.1042/BST20220830.
[10] E.G. Knox, M.R. Aburto, G. Clarke, J.F. Cryan, C.M. O’Driscoll, The blood-brain barrier in aging and neurodegeneration, Mol Psychiatry 27 (2022) 2659–2673. https://doi.org/10.1038/s41380-022-01511-z.
[11] F. Erdő, L. Denes, E. de Lange, Age-associated physiological and pathological changes at the blood-brain barrier: A review, J Cereb Blood Flow Metab 37 (2017) 4–24. https://doi.org/10.1177/0271678X16679420.
[12] J. Wen, Y. Ding, L. Wang, Y. Xiao, Gut microbiome improves postoperative cognitive function by decreasing permeability of the blood-brain barrier in aged mice, Brain Res Bull 164 (2020) 249–256. https://doi.org/10.1016/j.brainresbull.2020.08.017.
[13] L. Qi, F. Wang, X. Sun, H. Li, K. Zhang, J. Li, Recent advances in tissue repair of the blood-brain barrier after stroke, J Tissue Eng 15 (2024) 20417314241226551. https://doi.org/10.1177/20417314241226551.




Comments (0)
There are no comments for this article. Be the first one to leave a message!