Methylene blue is a synthetic compound first discovered in the 19th century and was initially used as a textile dye. Its medical applications became apparent soon after, particularly as an anti-malarial agent and a biological stain. Over the years, methylene blue has proven valuable across multiple therapeutic areas, including detoxification processes. Its unique properties, including electron exchange capabilities and mitochondrial support, make it a promising candidate for mitigating toxic effects in the body.
In today’s article, we will explore the mechanisms, applications, and safety considerations of methylene blue in different scenarios relating to detoxification, drawing from its established use in clinical and experimental settings.
Chemical and Biological Properties of Methylene Blue
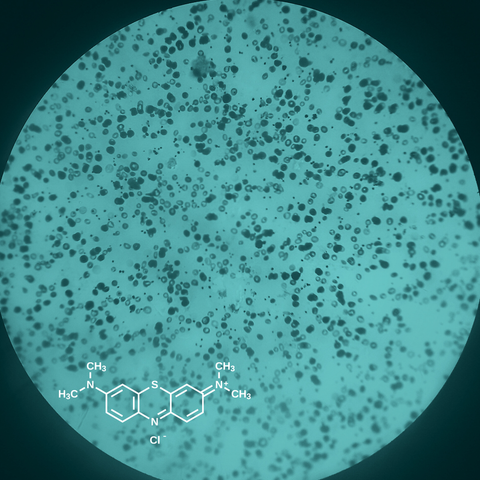
Methylene blue belongs to the thiazine dye family and exhibits high solubility in water and lipids, allowing it to cross cell membranes easily. As a redox-active compound, it alternates between oxidized (blue) and reduced (colorless) states. This redox cycling is central to its therapeutic action.
Commercially, methylene blue synthesis is accomplished via the oxidation of N,N-dimethyl-phenylenediamine with sodium dichromate in the presence of sodium thiosulfate, followed by further oxidation in the presence of N,N-dimethylaniline. Considered the first synthetic medication used in humans [1], it is an odorless dark green crystalline powder that becomes a blue solution when mixed with water. Its first uses in medicine were as an intestinal and urinary antiseptic and weak antimalarial agent [2].
Methylene blue is rapidly distributed into the brain, lungs, heart, liver, and kidneys. It is eliminated in urine, bile, and feces as leukomethylene blue. It has diverse uses in medicine including those for medical procedures, such as identifying the ureters in urological surgery and the gland in parathyroid surgery, and as a treatment for poisonings. Interestingly, methylene blue is known in oncologic literature to be an effective treatment for the reversal of ifosfamide-induced encephalopathy. In the 1990s, methylene blue was also studied in vasoplegic shock and was noted to improve blood pressure in patients. We will discuss a select few of these applications below.
Methylene Blue and Methemoglobinemia
In 1933, methylene blue was first used to treat aniline-induced methemoglobinemia (MetHB) [2,3]. Methemoglobinemia is a disorder of red blood cells that can be hereditary or acquired. In this disorder, the hemoglobin molecule (the oxygen carrier in blood) is adversely affected by the oxidation of iron (Fe).
Methemoglobin forms when the iron atom in the hemoglobin molecule is oxidized from ferrous to ferric iron. Only the ferrous iron can bind and release oxygen. Methylene blue is an oxidizing agent and in the presence of nicotinamide adenine dinucleotide phosphate (NADPH) is converted to leukomethylene blue. Leukomethylene blue then reduces methemoglobin to hemoglobin. Methemoglobin has a strong affinity for its bound oxygen atom, causing a leftward shift in the oxygen dissociation curve, resulting in the decreased release of oxygen at the tissue level. Methemoglobin is normally present in very low concentrations in the body but is considered abnormal if there is greater than 1% concentration.
Methylene blue is commonly employed in the treatment of methemoglobinemia as a first-line agent, and it works through its conversion to leukomethylene blue by NADPH, which then allows the reduction of MetHB to hemoglobin.
Methylene Blue and Mitochondrial Toxins or Toxicity
Cyanide is one of the most feared mitochondrial poisons and represents a significant source of intoxication in victims of smoke inhalation. In cells, cyanide inhibits cytochrome c oxidase, a crucial protein complex in oxidative phosphorylation (the process cells use to metabolize nutrients using oxygen). In simple terms, cyanide poisoning causes cells to asphyxiate [4].
In tropical regions of Africa, high intake of cyanide from the cassava plant has been linked to outbreaks of spastic paralysis with myoclonus. The optimal treatment strategy for people with cyanide intoxication is still debated, relying on addressing symptoms and providing antidotes. These antidotes are aimed at scavenging free cyanide and/or increasing cyanide elimination as thiocyanate using sodium thiosulfate.
In 1932, the first clinical report of the antidotal properties of methylene blue against cyanide poisoning was published [5]. A young man who had ingested “15 grains of potassium cyanide in 4 ounces of water," was admitted to the San Francisco Hospital. While comatose, he was given an aqueous solution of methylene blue and regained consciousness within five minutes and “fully” recovered within fifteen minutes. Other experimental observations obtained in vitro and in vivo suggested that methylene blue could antagonize cyanide toxicity, spurring a controversy on the mechanisms of its antidotal properties [6,7]. A 2018 study in rodents showed that methylene blue administered at the same time as potassium cyanide restored blood pressure, cardiac contractility, and limited oxygen deficit, allowing all the animals to survive without any significant methemoglobinemia [5]. When administered five minutes after a non-lethal cyanide intoxication, methylene blue accelerated the recovery of lactate and oxygen deficit. Finally, methylene blue was able to decrease the production of reactive oxygen species and restore the ATP/ADP ratio.
Methylene Blue and Chemotherapy-Related Detoxification
Cisplatin is a platinum-based cytostatic drug that is widely used for cancer treatment. Mitochondria and mitochondrial DNA (mtDNA) are important targets for platinum-based cytostatics, which mediates its nephrotoxicity (toxicity to the kidneys).
It is important to develop therapeutic approaches to protect the kidneys from cisplatin during chemotherapy. In both in vivo and in vitro experiments, cisplatin has been shown to cause strong damage to renal mtDNA [8]. Cisplatin injections cause oxidative stress by depleting renal (i.e., renal) antioxidants at the transcriptome level. In brief, methylene blue can cause an increase in the expression of genes involved in mtDNA repair and antioxidant defense, illustrating its protective effect. These findings potentially highlight the promise of methylene blue as a protective agent for the kidneys in the event of cisplatin-associated damage.
Ifosfamide is a chemotherapeutic agent, which is a synthetic analog of cyclophosphamide [9,10]. Side effects of ifosfamide can include hair loss, bladder irritation, and central nervous system (CNS) toxicity. The neurological toxicities include encephalopathy, lethargy, and personality changes. During the metabolism of ifosfamide, chloroacetaldehyde is produced, which is a potentially neurotoxic metabolite that crosses the blood-brain barrier and has been suggested as the mechanism underlying ifosfamide encephalopathy.
The incidence of CNS toxicity following ifosfamide therapy is estimated between 10 to 20%. High doses of ifosfamide are associated with higher rates of adverse effects, however, encephalopathy can be demonstrated at any dose and specific blood levels of ifosfamide have not been clearly linked to the development of neurotoxicity. Current guidelines for ifosfamide encephalopathy include treatment cessation, supportive care, and the use of methylene blue as a therapeutic and prophylactic treatment. The mechanism of methylene blue in this regard involves the inhibition of monoamine oxidase, which is involved in chloroacetaldehyde formation. It is effective within 30 minutes and can last up to three days [9].
Additionally, methylene blue has various applications in breast cancer, such as in sentinel lymph node biopsies. You can read more here.
Conclusion
Methylene blue is a versatile compound with profound implications for detoxification. Its ability to enhance mitochondrial function, neutralize oxidative stress, and modulate inflammation underpins its therapeutic potential.
This article has discussed several applications for methylene blue in a detoxifying capacity, firstly in its role as a prominent treatment for methemoglobinemia. We also explored its protective effect on kidney mitochondrial DNA during cisplatin chemotherapy and its neuroprotective role during ifosfamide treatment.
Methylene blue clearly offers much promise as a detox agent, but further research is necessary to fully clarify its mechanisms and optimize its applications whilst ensuring safety.
References
[1] B.K. Saha, S.L. Burns, The Story of Nitric Oxide, Sepsis and Methylene Blue: A Comprehensive Pathophysiologic Review, Am J Med Sci 360 (2020) 329–337. https://doi.org/10.1016/j.amjms.2020.06.007.
[2] R.S. Pushparajah Mak, E.L. Liebelt, Methylene Blue: An Antidote for Methemoglobinemia and Beyond, Pediatr Emer Care 37 (2021) 474–477. https://doi.org/10.1097/PEC.0000000000002526.
[3] A. Skold, D.L. Cosco, R. Klein, Methemoglobinemia: pathogenesis, diagnosis, and management, South Med J 104 (2011) 757–761. https://doi.org/10.1097/SMJ.0b013e318232139f.
[4] G. Doman, J. Aoun, J. Truscinski, M. Truscinski, S. Aouthmany, Cyanide Poisoning, J Educ Teach Emerg Med 7 (2022) S1–S25. https://doi.org/10.21980/J80W76.
[5] P. Haouzi, M. Gueguinou, T. Sonobe, A. Judenherc-Haouzi, N. Tubbs, M. Trebak, J. Cheung, F. Bouillaud, Revisiting the physiological effects of methylene blue as a treatment of cyanide intoxication, Clin Toxicol (Phila) 56 (2018) 828–840. https://doi.org/10.1080/15563650.2018.1429615.
[6] P. Haouzi, M. McCann, J. Wang, X.-Q. Zhang, J. Song, I. Sariyer, D. Langford, M. Santerre, N. Tubbs, A. Haouzi-Judenherc, J.Y. Cheung, Antidotal effects of methylene blue against cyanide neurological toxicity: in vivo and in vitro studies, Ann N Y Acad Sci 1479 (2020) 108–121. https://doi.org/10.1111/nyas.14353.
[7] P. Haouzi, M. McCann, N. Tubbs, A. Judenherc-Haouzi, J. Cheung, F. Bouillaud, Antidotal Effects of the Phenothiazine Chromophore Methylene Blue Following Cyanide Intoxication, Toxicol Sci 170 (2019) 82–94. https://doi.org/10.1093/toxsci/kfz081.
[8] N.A. Samoylova, A.P. Gureev, V.N. Popov, Methylene Blue Induces Antioxidant Defense and Reparation of Mitochondrial DNA in a Nrf2-Dependent Manner during Cisplatin-Induced Renal Toxicity, Int J Mol Sci 24 (2023) 6118. https://doi.org/10.3390/ijms24076118.
[9] G. Chain, M. Kalia, K. Kestenbaum, L. Pappas, A. Sechser-Perl, G.A. Campino, N. Zaghloul, A novel case of prolonged Ifosfamide encephalopathy and long-term treatment with methylene blue: a case report and review of literature, BMC Pediatr 22 (2022) 76. https://doi.org/10.1186/s12887-022-03144-1.
[10] A. Küpfer, C. Aeschlimann, T. Cerny, Methylene blue and the neurotoxic mechanisms of ifosfamide encephalopathy, Eur J Clin Pharmacol 50 (1996) 249–252. https://doi.org/10.1007/s002280050102.





Comments (0)
There are no comments for this article. Be the first one to leave a message!