GABA and gabapentin are two fundamentally different compounds that share some important similarities. The first, gamma- or γ-aminobutyric acid (or GABA), is a neurotransmitter that serves as a chemical messenger in the brain. The other, gabapentin, which you may also know as Neurontin, is a so-called analog of GABA, meaning that it was designed to mimic certain qualities of the neurotransmitter.
The goals of this article are to provide some background on each one as well as an overview of both their shared and unique qualities.
Chemical Structure and Composition
GABA is a naturally occurring neurotransmitter in the brain (i.e., organic). It is the primary inhibitory neurotransmitter in the cerebral cortex, with its main role being the reduction of neuronal excitability throughout the nervous system [1,2].
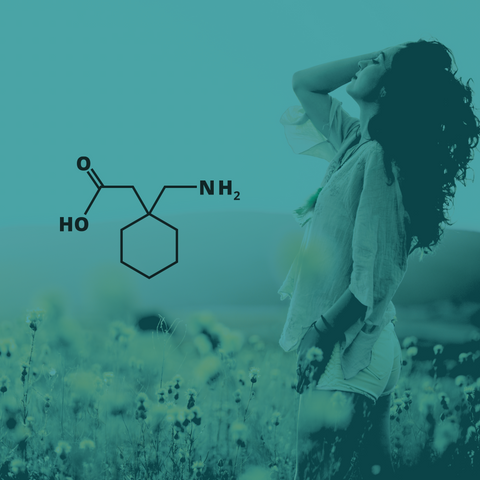
Conversely, gabapentin was first synthesized to be a GABA analog. However, gabapentin does not possess the same chemical composition or capacity as GABA. Gabapentin was designed to more readily cross the blood–brain barrier (BBB), in contrast to GABA, and its initial application was in the treatment of epilepsy [3].
Mechanisms of Action
GABA plays an important role in neuronal proliferation, migration, differentiation, and preliminary circuit-building during brain development. It also regulates connectivity between the major functional networks in the brain, such as the default mode and executive control networks [4]. GABA binds with two major post-synaptic receptors, the GABA-A and GABA-B receptors. The former is an ionotropic receptor that increases chloride ion conductance in the cell in the presence of GABA. The extracellular concentration of chloride is normally much higher than the intracellular concentration. Consequently, the influx of negatively charged chloride ions hyperpolarizes the cell, inhibiting the creation of an action potential. The GABA-B receptor functions via a metabotropic G-protein coupled receptor which increases postsynaptic potassium conductance and decreases presynaptic calcium conductance, which consequently hyperpolarizes the postsynaptic cell and prevents the conduction of an action potential in the presynaptic cell. As a consequence and irrespective of the GABA receptor type, GABA serves an inhibitory role [5].
For gabapentin, the exact mechanism of action with GABA receptors is unknown. However, researchers know that gabapentin freely passes the BBB and subsequently acts on neurotransmitters. Even though it has a similar structure to GABA, it does not bind to GABA receptors and does not influence the synthesis or uptake of GABA. Rather, gabapentin works by showing a high affinity for binding sites throughout the brain that correspond to the presence of voltage-gated calcium channels, especially alpha-2-delta-1, which seems to inhibit the release of excitatory neurotransmitters in the presynaptic area that participate in epileptogenesis. Even though there is no evidence for direct action at the serotonin, dopamine, benzodiazepine, or histamine receptors, research has shown gabapentin to increase levels of serotonin in the blood of healthy control subjects [6].
Major Effects and Uses
GABA is the major inhibitory neurotransmitter in the central nervous system (CNS) and it has been estimated that at least one-third of all CNS neurons utilize GABA as their primary neurotransmitter. GABAergic inhibition is essential for maintaining the balance between neuronal excitation and inhibition, for tight temporal and spatial control of transsynaptic signaling, temporal modulation of neuronal excitability, and maintaining oscillatory “pacemaker” activities in numerous brain regions. Most GABA-containing neurons are interneurons, which control the excitability of local circuits within a given brain region, although some major projection pathways – notably arising in the thalamus and cortex – are GABAergic [7]. Research suggests that GABA can improve mood and/or have a calming effect on the nervous system that can lessen anxiety and induce sleep, whereas low GABA levels are thought to drive anxiety or mood disorders, epilepsy, and chronic pain [8-10].
Gabapentin has principal uses as an anticonvulsant medication used for the treatment of partial seizures in adults and neuropathic pain (such as that caused by diabetic neuropathy, postherpetic neuralgia, and central pain). As such, gabapentin is a prescription medication. However, it has also been prescribed off-label in the United States and the United Kingdom for the treatment of non-neuropathic pain, anxiety, and bipolar disorder [11-13]. It is a prescribed first-line treatment for multiple sclerosis and for some types of nystagmus [14,15], as well as a potential option for restless legs syndrome [16].
Metabolism, Half-Life, and Common Side Effects
When taken in oral supplement form, GABA is rapidly absorbed (within 30 to 60 minutes) and has a half-life of around 5 hours [17]. However, most of the supplement is unlikely to reach the brain due to its inability to traverse the BBB.
After taking gabapentin, it is absorbed from the intestines by an amino acid transporter and, at low doses, reaches peak concentrations at around 2 hours [18]. The elimination half-life of gabapentin is 5 to 7 hours, and it takes two days for the body to eliminate gabapentin from its system [6,19,20]. One beneficial advantage of gabapentin use is its mild side-effect profile. The most often reported side effects of gabapentin are fatigue, dizziness, and headache. Although adverse effects occur in most patients receiving gabapentin as adjunctive therapy, they are transient and mild to moderate in severity. To date, serious adverse effects have been rare [21].
Summary
In this article, we have addressed the fundamental differences and similarities between GABA and its analog, gabapentin, from the standpoint of chemical structure, mechanism of action, metabolism, and side effect profile.
The similarities between GABA and gabapentin would be to highlight their shared effects on the nervous system (i.e., inhibition), their use in medicinal settings, and the potential for side effects.
The differences between GABA and gabapentin lie in their mechanisms of action in the brain – GABA targets GABA receptors whereas gabapentin interacts with voltage-gated calcium channels.
If you're interested in the modulation of your GABA system to your benefit and without risk of tolerance, withdrawal, or dependence, try Tro Calm and Tro Zzz, our buccal troches that help with anxiousness and sleep, respectively.
References
[1] W. Froestl, An historical perspective on GABAergic drugs, Future Med Chem 3 (2011) 163–175. https://doi.org/10.4155/fmc.10.285.
[2] L. Sivilotti, A. Nistri, GABA receptor mechanisms in the central nervous system, Prog Neurobiol 36 (1991) 35–92. https://doi.org/10.1016/0301-0082(91)90036-z.
[3] J.A. Dougherty, D.H. Rhoney, Gabapentin: a unique anti-epileptic agent, Neurol Res 23 (2001) 821–829. https://doi.org/10.1179/016164101101199414.
[4] A.J. Cutler, G.W. Mattingly, V. Maletic, Understanding the mechanism of action and clinical effects of neuroactive steroids and GABAergic compounds in major depressive disorder, Transl Psychiatry 13 (2023) 228. https://doi.org/10.1038/s41398-023-02514-2.
[5] X. Leinekugel, I. Khalilov, H. McLean, O. Caillard, J.L. Gaiarsa, Y. Ben-Ari, R. Khazipov, GABA is the principal fast-acting excitatory transmitter in the neonatal brain, Adv Neurol 79 (1999) 189–201.
[6] M. Chincholkar, Gabapentinoids: pharmacokinetics, pharmacodynamics and considerations for clinical practice, Br J Pain 14 (2020) 104–114. https://doi.org/10.1177/2049463720912496.
[7] P. Nuss, Anxiety disorders and GABA neurotransmission: a disturbance of modulation, Neuropsychiatr Dis Treat 11 (2015) 165–175. https://doi.org/10.2147/NDT.S58841.
[8] S. Yang, B. Zhang, D. Wang, S. Hu, W. Wang, C. Liu, Z. Wu, C. Yang, Role of GABAergic system in the comorbidity of pain and depression, Brain Research Bulletin 200 (2023) 110691. https://doi.org/10.1016/j.brainresbull.2023.110691.
[9] Y. Cruz-Almeida, M. Forbes, R.C. Cohen, A.J. Woods, R.B. Fillingim, J.L. Riley, E.S. Porges, Brain gamma-aminobutyric acid, but not glutamine and glutamate levels are lower in older adults with chronic musculoskeletal pain: considerations by sex and brain location, Pain Rep 6 (2021) e952. https://doi.org/10.1097/PR9.0000000000000952.
[10] Y. Feng, Z.-H. Wei, C. Liu, G.-Y. Li, X.-Z. Qiao, Y.-J. Gan, C.-C. Zhang, Y.-C. Deng, Genetic variations in GABA metabolism and epilepsy, Seizure: European Journal of Epilepsy 101 (2022) 22–29. https://doi.org/10.1016/j.seizure.2022.07.007.
[11] F. Montastruc, S.Y. Loo, C. Renoux, Trends in First Gabapentin and Pregabalin Prescriptions in Primary Care in the United Kingdom, 1993-2017, JAMA 320 (2018) 2149–2151. https://doi.org/10.1001/jama.2018.12358.
[12] A.M. Peckham, K.E. Evoy, L. Ochs, J.R. Covvey, Gabapentin for Off-Label Use: Evidence-Based or Cause for Concern?, Subst Abuse 12 (2018) 1178221818801311. https://doi.org/10.1177/1178221818801311.
[13] H. McAnally, U. Bonnet, A.D. Kaye, Gabapentinoid Benefit and Risk Stratification: Mechanisms Over Myth, Pain Ther 9 (2020) 441–452. https://doi.org/10.1007/s40122-020-00189-x.
[14] R.J. McLean, I. Gottlob, The pharmacological treatment of nystagmus: a review, Expert Opin Pharmacother 10 (2009) 1805–1816. https://doi.org/10.1517/14656560902978446.
[15] A.R. Mehta, C. Kennard, The pharmacological treatment of acquired nystagmus, Pract Neurol 12 (2012) 147–153. https://doi.org/10.1136/practneurol-2011-000181.
[16] J. Winkelmann, R.P. Allen, B. Högl, Y. Inoue, W. Oertel, A.V. Salminen, J.W. Winkelman, C. Trenkwalder, C. Sampaio, Treatment of restless legs syndrome: Evidence-based review and implications for clinical practice (Revised 2017)§, Mov Disord 33 (2018) 1077–1091. https://doi.org/10.1002/mds.27260.
[17] J. Li, Z. Zhang, X. Liu, Y. Wang, F. Mao, J. Mao, X. Lu, D. Jiang, Y. Wan, J.-Y. Lv, G. Cao, J. Zhang, N. Zhao, M. Atkinson, D.L. Greiner, G.J. Prud’homme, Z. Jiao, Y. Li, Q. Wang, Study of GABA in Healthy Volunteers: Pharmacokinetics and Pharmacodynamics, Front Pharmacol 6 (2015) 260. https://doi.org/10.3389/fphar.2015.00260.
[18] E.P. Calandre, F. Rico-Villademoros, M. Slim, Alpha2delta ligands, gabapentin, pregabalin and mirogabalin: a review of their clinical pharmacology and therapeutic use, Expert Rev Neurother 16 (2016) 1263–1277. https://doi.org/10.1080/14737175.2016.1202764.
[19] M.J. McLean, Clinical pharmacokinetics of gabapentin, Neurology 44 (1994) S17-22; discussion S31-32.
[20] A. Beydoun, B.M. Uthman, J.C. Sackellares, Gabapentin: pharmacokinetics, efficacy, and safety, Clin Neuropharmacol 18 (1995) 469–481.
[21] R.E. Ramsay, Clinical efficacy and safety of gabapentin, Neurology 44 (1994) S23-30; discussion S31-32.





Comments (0)
There are no comments for this article. Be the first one to leave a message!